Nailfold Capillaroscopy
Last updated: February 23, 2015
Synonym: Wide-field nailfold capillaroscopy.
Description: Easily performed, this test examines nailfold capillary architecture by microscopy. Although not truly specific, the test is useful in distinguishing primary and secondary Raynaud’s phenomenon. Secondary Raynaud disease refers to Raynaud phenomenon in the setting of another connective tissue disorder (e.g., systemic sclerosis, CREST syndrome, RA, or SLE).
Method: A clean nailbed from the third and fourth (preferred) fingers should be examined at room temperature using low-power magnification from either an ophthalmoscope (+40 diopters), hand-held illuminating microscope (10–40X, available from Radio Shack), or a wide-field stereomicroscope (12–14X) using a low-voltage lamp that does not heat the skin. Videomicroscopy has also been used. Place a drop of grade B immersion oil, mineral oil, or lubricant gel (e.g., K-Y Jelly) proximal to the cuticle. Look for evenly arranged capillary loops arising from the nailbed with a hairpin appearance. There may be finger to finger variation.
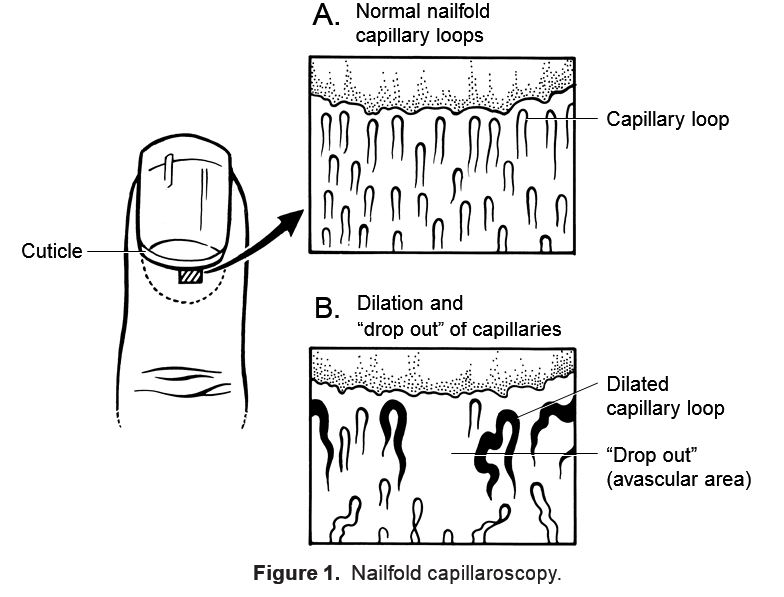
Normal: Normal vessels are thin, uniform, evenly spaced, and symmetric in distribution (Fig. 1). Normal capillary loops have a hairpin appearance. Normal vessels are seen in most rheumatic disorders, including fibromyalgia, osteoarthritis, gout, primary Raynaud phenomenon, and eosinophilic fasciitis. Minor vessel abnormalities and a few avascular areas are uncommonly seen in normal individuals. However, extensive hemorrhage and avascular dropout and bizarre or giant vessels are rarely seen in normal controls.
Abnormal: Commonly seen abnormalities may include absent (“dropout” areas) or dilated capillary loops. Vessel architecture may be described as irregular, tortuous, elongated, bizarre, bushy, engorged, or corkscrew in appearance. Spacing between loops may be uneven or irregular (Fig. 1).
—Primary Raynaud phenomenon: Normal capillaries are most common and suggest a good prognosis and low risk of future development of scleroderma and related disorders.
—Scleroderma: The scleroderma pattern (also seen with CREST and mixed connective tissue disease) is one of enlarged or dilated capillary loops with areas of intervening vessel dropout. Dropout is specific for scleroderma. Tortuous vessels, distortion, or “budding” of capillaries may be seen. Capillary hemorrhages and bizarre vessel architecture are common. The extent of capillary lesions may correlate with the severity of end-organ damage and survival rates.
—Dermatomyositis: Patients with dermatomyositis are frequently abnormal, with vessel changes similar to scleroderma. Giant, engorged vessels with hemorrhage may be seen macroscopically. Patients with SLE may be abnormal with corkscrew-appearing capillaries.
—Others: Nailfold capillary abnormalities have also been described in patients with diabetes mellitus, RA, psoriasis, and Behçet’s syndrome.
Indications: Nailfold capillaroscopy is useful as a bedside aid to the differential diagnosis of Raynaud’s phenomenon or an undifferentiated connective tissue disease. Many undifferentiated patients with abnormal capillary find- ings progress to a fully manifest syndrome. Capillaroscopy may be of some value in documenting the extent of microvascular disease in patients with scleroderma, CREST, mixed connective tissue disease, and dermatomyositis.
Cost: Inexpensive; procedure takes 3–5 minutes to perform using an ophthalmoscope, hand-held microscope, or dermatoscope (Fig. 1).